|
|
|
|
|
Reproductive System Navigation links Sexual reproduction is the process of producing offspring for the survival of the species, and passing on hereditary traits from one generation to the next. The male and female reproductive systems contribute to the events leading to fertilization. Then, the female organs assume responsibility for the developing human, birth, and nursing. The male and female gonads (testes and ovaries) produce sex cells (ova and sperm) and the hormones necessary for the proper development, maintenance, and functioning of the organs of reproduction and other organs and tissues.
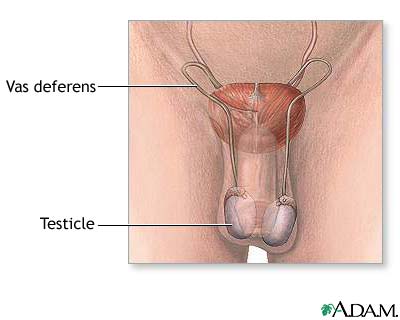
The reproductive system comprises the reproductive organs. In the male, the organs include the testes, accessory ducts, accessory glands, and penis. In the female, the organs include the uterus, uterine tubes, ovaries, vagina, and vulva. The testes are paired reproductive organs in the scrotum, which hangs outside the human body. Normal sperm production requires the cooler outside temperature. Each testis contains coiled seminiferous tubules where sperm (male reproductive cells) production occurs. Between the seminiferous tubules are Leydig cells, clusters of endocrine (secretory) cells. Leydig cells produce androgens (sex hormones), mostly testosterone.
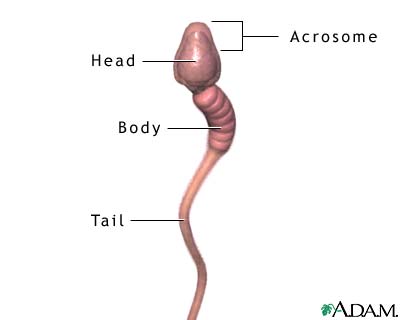
Each sperm cell has three parts: a head, middle piece, and tail. An acrosome at the head tip produces enzymes that help penetrate the female ovum (egg). During conception, chromosomes (genetic material) in the nucleus (cell control center) join with chromosomes in the ovum. The middle piece contains mitochondria, structures that provide energy for the sperm. The mitochondria are tightly spiraled around the axial filaments (contractile portion) of the flagellum (tail). Centrioles form the tail, which moves the sperm toward the ovum. An ejaculation (ejection of sperm from the penis) has 300 to 500 million sperm. The accessory ducts store secretions from the testes and accessory glands and deliver secretions to the penis. The epididymis, a coiled tube next to each testis, receives sperm from the seminiferous tubules. The epididymis has three parts: a head, body, and tail. The epididymis stores sperm and propels it toward the penis. Smooth muscle contractions in the epididymis walls move sperm through the duct. As sperm pass through the epididymis, the sperm mature and receive nourishment.
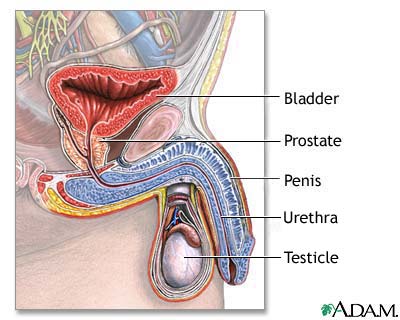
The vas deferens is the dilated continuation of the epididymis. The vas deferens travels out of the scrotum and into the abdomen (gut cavity) through the inguinal canal. Once in the abdomen, the vas deferens passes behind the urinary bladder and expands to form an ampulla (expanded end part). Each ampulla joins with a seminal vesicle (an accessory gland) to form an ejaculatory duct. The vas deferens is the main sperm carrier. Its walls contain three layers of smooth muscle innervated by sympathetic nerves. Stimulation of these nerves propels sperm into the ejaculatory ducts. Here, the ampulla of the vas deferens and seminal vesicles meet and secretions from the seminal vesicles and sperm are stored. From this junction, the ejaculatory ducts pass through the prostate gland, where they receive more secretions, then join with the single urethra (tube through which sperm and urine pass out of body). The urethra is the final section of the duct system. It passes from the urinary bladder and the ends of the ejaculatory ducts through the prostate gland and into the penis. The urethra receives secretions from the ejaculatory ducts, the prostate gland, and the bulbourethral glands (accessory glands). The urethra carries sperm through the penis during intercourse; during urination, urine passes through it. The urethra cannot execute both functions simultaneously. During ejaculation, a muscular sphincter (ring of muscle) closes off the bladder.
The accessory glands produce fluids that nourish and energize the sperm for the journey to the ovum. For example, during sexual excitement the seminal vesicles add secretions to the sperm in the ejaculatory duct. These secretions provide energy for the sperm and a neutralizing chemical that reduces vaginal acidity. The prostate gland lies under the urinary bladder and surrounds the first part of the urethra. Its secretions also help neutralize vaginal acidity and make sperm motile (able to move). The bulbourethral glands secrete a clear fluid that neutralizes the acidity of remaining urine in the urethra. When secretions of these glands combine with sperm, the result is seminal fluid, or semen. Only 1 percent of semen is sperm. The remainder contains fructose to nourish the sperm, an alkaline component to neutralize vaginal and urethral acidity, and salts and phospholipids, substances that make sperm motile. The penis (male sexual organ) deposits semen into the vagina during sexual intercourse and carries urine through the urethra during urination. It contains erectile tissue that becomes engorged with blood during sexual excitement, resulting in an erection. The penis includes the shaft (tubular portion), glans (penis tip and sexual sensation center), and the prepuce, or foreskin (loose skin fold over glans). In a circumcision procedure, the prepuce is removed. The female reproductive system is more complex than that of the male. It produces ova (egg cells); nourishes, carries, and protects the developing embryo; and nurses the newborn after birth. The system structures are the ovary, uterine tubes, uterus, vagina, vulva, and mammary glands.
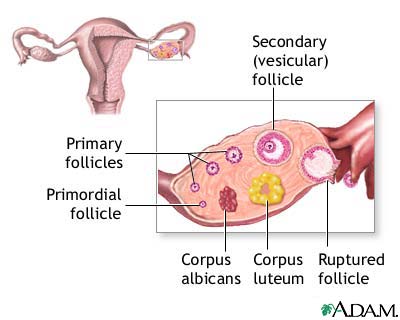
Ovaries, a pair of female gonads (sex organs), reside in the pelvic part of the abdomen on either side of the uterus. Ovaries produce ova and estrogen (female sex hormone). At puberty onset, the menstrual (uterine) cycle, a series of cyclic changes to the endometrium (uterine lining) begins. The ovarian cycle, fluctuating levels of ovarian hormones in the blood, causes the menstrual cycle. The ovarian and menstrual cycles begin each month when a follicle (developing ovum surrounded by a cluster of cells) develops in the ovary. The hypothalamus in the brain produces hormones that cause these cycles. The hypothalamus releases gonadotropin-releasing hormone (GnRH), which acts on the anterior pituitary gland. GnRH causes the pituitary to release two more hormones: follicle-stimulating hormone (FSH) and luteinizing hormone (LH). FSH causes the primary oocyte within the follicle to develop into a secondary oocyte. Development occurs through meiosis (cell division that reduces the chromosome number in the cell from 46 to 23). Each secondary oocyte completes this division only when sperm fertilizes it. The developing follicle produces estrogen, which causes the endometrium to prepare to nourish a fertilized egg. Estrogen also inhibits pituitary gland production of FSH. The elevated estrogen level causes the anterior pituitary to release LH. This action causes ovulation, a process in which the follicle rapidly enlarges and releases the secondary oocyte. LH also causes the collapsed follicle to become the corpus luteum, an endocrine (secretory) body. The corpus luteum secretes estrogen and progesterone (hormone that stimulates endometrium thickening). These hormones complete the endometrium development and maintain the endometrium for 10 to 14 days.
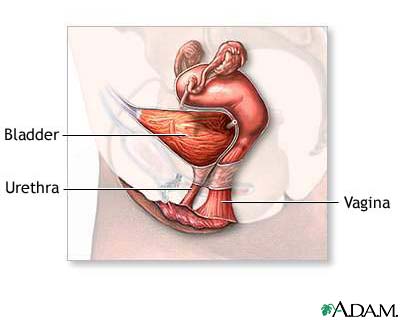
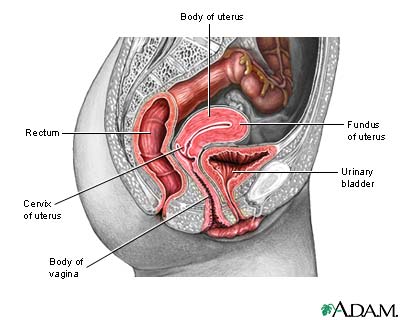
Unless sperm fertilize the secondary oocyte, the corpus luteum begins to degenerate, dropping blood progesterone levels. Without progesterone to maintain the endometrial lining, the lining is shed with the degenerated oocyte approximately 14 days after ovulation. After ovulation, estrogen and progesterone act in the bloodstream to inhibit anterior pituitary production of LH and FSH. This negative feedback control ensures that only one follicle develops each cycle. Each cycle lasts approximately 28 days. The uterine tubes (oviducts or fallopian tubes) are paired tubes that receive the developing ovum from the ovary. The infundibulum end is beside the ovary; its fimbria (feathery structures) "sweep" the developing ovum into the tube. The ampulla, the middle part of the uterine tube, contains smooth muscle to move the egg. Cilia (inner wall little projections) also sweep the egg along the tube. The unfertilized ovum degenerates in the ampulla; the fertilized ovum resumes its journey to the uterus. The isthmus end of the uterine tube opens into the uterus. The uterus is a hollow muscular organ in front of the rectum and behind the urinary bladder. The fundus is the wide upper portion. The body is the tapered middle part that ends at the cervix (junction between the vagina and uterus). The isthmus is the constricted region between the body and cervix. The round ligaments hold the uterus anteverted (inclined forward) over the urinary bladder.
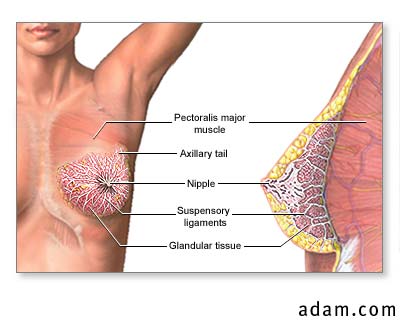
The uterus has three layers. The outer serous layer forms ligaments that hold it to the pelvic walls. The middle muscular layer has three muscle layers used in labor to deliver a baby. The endometrium inner mucosal lining has two layers, the stratum functionalis and stratum basalis. Every month the stratum functionalis is built up in response to estrogen secretion. It contains blood vessels and glands to nourish the fertilized ovum. Unless sperm fertilizes the secondary oocyte, the corpus luteum disintegrates into corpus albicans, and estrogen and progesterone secretion cease. Without these hormones, the endometrium breaks down and menstruation (expulsion of endometrial lining from the uterus through the vagina) occurs. After menstruation, progesterone and LH levels decrease. The inhibition of LH causes the anterior pituitary to secrete FSH, which stimulates development of another ovum. The monthly cycle begins again. The vagina is a muscular tube from the uterus to outside the body. In some women, the hymen (thin tissue) partially covers the vaginal orifice. Initial sexual intercourse or other form of penetration ruptures the hymen. The vagina receives sperm from sexual intercourse, channels menstrual flow out of the body, and is a birth canal for the baby during childbirth. Normally collapsed, it can enlarge to accommodate an erect penis or a birth. The vulva, external genitalia, includes the mons pubis, labia majora, labia minora, and clitoris. The mons pubis is a mound of fatty tissue at the junction of the thighs and torso. During puberty, pubic hair covers it. The labia majora are skin folds that form the vulva outer border. During puberty, pubic hair covers the labia majora, too. The labia minora are inner, smaller skin folds that surround the urethral and vaginal openings. The labia minora merge anteriorly to form the prepuce (foreskin) of the clitoris. This small erectile structure, comparable to the male penis, becomes engorged with blood during sexual excitement and is the female center of sexual sensation. The mammary glands have 15 to 20 lobes of glandular tissue. The lobes contain lactiferous ducts that converge toward the nipple. These ducts dilate just before they reach the lactiferous sinus, then constrict again before passing out of the nipple through 15 to 20 openings.
The mammary glands are in the breasts. These glands overlie the pectoral muscles and are attached to them via fascia (connective tissue). The glands are connected to the skin by the suspensory ligaments of the breast. These glands are modified sweat glands that produce and secrete milk during the lactation process to feed the newborn. During pregnancy, high blood estrogen and progesterone levels stimulate lactation. The corpus luteum produces these hormones during early pregnancy; the placenta takes over later. The hormones stimulate the ducts and glands in the breasts, enlarging the breasts. The formation of sex cells begins before birth; spermatozoa form in males and oocytes in females. Spermatogenesis (sperm cell production) occurs in the seminiferous tubules. Spermatogonia (stem cells) line these tubules at birth and contain 46 chromosomes (genetic material). After birth, spermatogonia continue to divide during mitosis. This cell division process produces two daughter cells with the same chromosome number (46) as the parent. At puberty onset, some spermatozoa grow to become primary spermatocytes. These cells undergo meiosis, the cell division process that cuts back the number of chromosomes from 46 to 23. Each primary spermatocyte undergoes the first meiotic division to produce two secondary spermatocytes. Each secondary spermatocyte undergoes the second meiotic division to produce two spermatids. Each spermatid develops into a mature spermatozoon (sperm cell). In this way, meiosis produces millions of sperm every day. Oogenesis is the formation of the ovum (female sex cells), which begin as hundreds of thousands of oogonia (stem cells) in the fetal ovaries. During prenatal development, the oogonia grow to become primary oocytes that contain 46 chromosomes. Each oocyte undergoes meiosis; at birth, oocytes are in prophase. During this first meiotic division, oocytes enter a resting phase that lasts until the oocyte resumes development during the ovarian cycle (puberty). The female is born with all the oocytes she will ever have. |
Any duplication or distribution of the information contained herein is strictly prohibited. The information provided herein should not be used for diagnosis or treatment of any medical condition and is provided for your general information only.