How systemic racism affects public health
Part 1: Health disparities among Black people
Edited by Emily Ornberg
Clinically reviewed by Chet Robson DO, MHCDS, FAAFP

As the nation reckons with racism, medical communities are taking action to address the health disparities among minorities—by declaring racism as a public health crisis.
While racism impacts all people of color, Black Americans have historically been among the most impacted. In this series, we'll look at some of the connections between race, racism and health in the United States and discuss actions toward health equity for all.
What is racism?
While it might seem obvious, the definition of "racism" has evolved—it doesn't just refer to hate groups or bigoted comments. Racism is folded into the foundation of our country—so much so, that racism may go unseen to some who don't experience it. Racism can be direct or indirect, and affects Black people, and other minorities—of all classes, ages and genders.
Here's how Camara Phyllis Jones, MD, MPH, PhD of the American Public Health Association (APHA) defines racism:
"Racism is a system of structuring opportunity and assigning value based on the social interpretation of how one looks (which is what we call "race"), that unfairly disadvantages some individuals and communities, unfairly advantages other individuals and communities, and saps the strength of the whole society through the waste of human resources."1
How is racism linked to public health?
Our race impacts our health outcomes, similar to other social determinants of health such as housing, education and work situations.1 Black Americans report higher overall stress levels compared to white Americans—and chronic, sustained stress over time can raise the risk for conditions such as heart disease, high blood pressure and depression.2 And lack of adequate health insurance coverage remains a major barrier to accessing quality health care for people of color and low-income individuals.3
The American Academy of Pediatrics, American Medical Association and American College of Physicians, among many other health institutions, have spoken out against the major health and socioeconomic disparities among Black Americans—naming racism as a public health concern.

The results are staggering—Black Americans are:
- 1.7 times more likely to be hospitalized4
- 2.2 times more likely to die as infants5
- 80 percent more likely to be diagnosed with diabetes6
- Up to 60 percent more likely to have high blood pressure7
- 40 percent more likely to die of breast cancer8
- 20 percent more likely to have visual impairments6
- 20 percent more likely to report psychological distress9
- 50 percent less likely to receive counseling or mental health treatment9
Overall, Black Americans are living longer, but in certain regions of the country, this isn't the case. For example, in Chicago in the predominately white and affluent neighborhood Streeterville, residents are expected to live until 90, while in the predominately Black and poor area Englewood (only nine miles away on the city's South Side) residents typically live until about 60, according to a study by NYU School of Medicine.10 The life expectancy for Blacks living in other cities is shorter, including LA County, New York City, and Washington D.C.
Black Americans are also more likely to have chronic health conditions, according to the CDC.11 Younger Black Americans are living with diseases more associated with older age groups, including high blood pressure, diabetes and stroke.
How has COVID-19 impacted races?

The COVID-19 pandemic has made race disparities—and the systematic racism they are rooted in—more apparent.
Severe illness and death rates have historically been higher for racial and ethnic minority groups during public health emergencies. To address the needs of these populations in emergencies, the CDC stresses improving their daily life and harnessing their strengths.12
What are some factors of these health disparities?
Various factors and social inequities have put some members of racial and ethnic minority groups at increased health risks. All of these factors affect our health, and all are shaped by systemic racism.
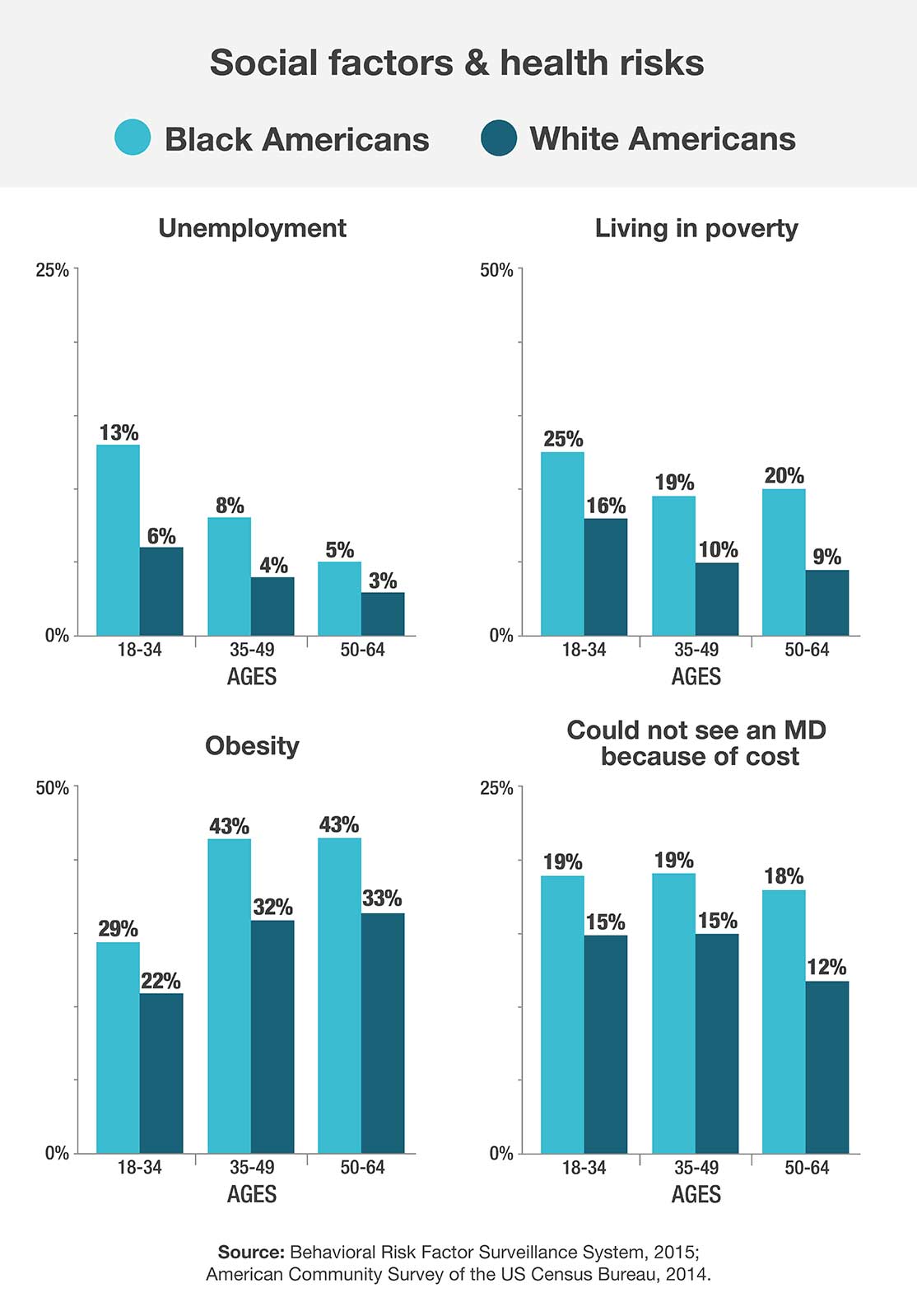
Black people are more likely than white people to:
- Report not being able to see a doctor in the past year because of cost
- Live in areas without clean water or air
- Have less access to green spaces
- Grow up in high-poverty areas
- Live in food deserts with limited access to fresh fruit or vegetables
- Be exposed to greater occupational hazards, often working in frontline jobs across many fields
What can be done
The first step is identifying racism a health crisis. Then comes a plan of action for addressing it.
The CDC recommends these actions for public healthcare providers.11
- Ensure healthcare professionals understand cultural differences and the social and economic conditions that may put some patients at higher risk than others.
- Link more people to accessible doctors, nurses or community health centers to encourage regular and follow-up medical visits.
- Support actions to create healthy food environments and increase physical activity in underserved communities.
What you can do
By discussing actions of racism with friends, coworkers and family, you are more likely to affect change in your communities.
- Address racist attitudes/ statements when you hear them.
- If you have the means, contribute to community organizations.
- Volunteer at organizations to help minorities gain better access care.
How Walgreens can help bridge access to care
To ensure everyone has the opportunity to be as healthy as possible, it's important to bridge access to care. Pharmacists are often the most accessible and frequently visited members of the healthcare team, especially in underserved areas.
We can help:
- Find affordable prescription drug coverage if you've lost insurance due to COVID-19.
- Locate clinics in your area at some of our 9,200 stores nationwide.
- Chat with a pharmacist 24/7.
- Get your prescriptions delivered.
- Schedule telehealth appointments for general illnesses, dermatology and mental health.
Entrenched health disparities impact the wellbeing of the Black community. As a healthcare resource in many communities, Walgreens is here to address and decrease those disparities. In Part 2, we will take a look at the differences in chronic conditions by race.
Published on July 29, 2020
Sources:
1. https://www.apha.org/topics-and-issues/health-equity/racism-and-health
2. https://www.mayoclinic.org/healthy-lifestyle/stress-management/in-depth/stress/art-20046037
4. http://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=18
5. http://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=23
6. http://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=18
7. http://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=19
8. http://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=16
9. http://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=24
10. https://apnews.com/cb4fbcf64546426d9de694ea5cf9f885
11. https://www.cdc.gov/vitalsigns/aahealth/index.html
12. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/racial-ethnic-minorities.html
13. https://pediatrics.aappublications.org/content/144/2/e20191765
14. https://www.ama-assn.org/about/leadership/police-brutality-must-stop
16. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1854988/
18. https://www.census.gov/newsroom/releases/archives/2010_census/cb11-cn185.html
20. https://www.lung.org/clean-air/outdoors/who-is-at-risk/disparities
21. https://www.nami.org/Your-Journey/Identity-and-Cultural-Dimensions/Black-African-American
22. https://www.samhsa.gov/data/report/2018-nsduh-detailed-tables
23. https://www.mhanational.org/issues/black-and-african-american-communities-and-mental-health
24. https://www.census.gov/content/dam/Census/library/publications/2019/demo/p60-266.pdf
26. http://www.equality-of-opportunity.org/assets/documents/race_summary.pdf
27. https://www.nationalpartnership.org/our-work/health/reports/black-womens-maternal-health.html
28. http://publichealth.lacounty.gov/epi/docs/Life%20Expectancy%20Final_web.pdf
29. https://www1.nyc.gov/site/doh/about/press/pr2019/fewer-premature-deaths-and-births.page
30. https://dcist.com/story/16/07/05/life-expectancy/
31. https://www.aafp.org/about/policies/all/institutional-racism.html
32. https://www.rutgers.edu/news/police-use-fatal-force-identified-leading-cause-death-young-men