Women's Health - Online Diagnoses & Prescriptions | Walgreens
Women’s health
We’re here to support your wellness journey with answers to your questions, expert advice, in-store services and recommended solutions.

Birth control, explained
What is birth control?
Birth control, also called contraception, refers to any medicine, method, or device a person uses to prevent pregnancy. Examples include combination oral contraception pills, progestin-only oral contraception pills, transdermal patches, transvaginal rings, diaphragms and condoms. Not all birth control methods are equally effective, and not all prevent the spread of sexually transmitted infections. A healthcare provider can help you decide which birth control method is best for you.
What are the types of birth control?
There are various types of birth control methods:
Reversible methods:
An intrauterine contraception device (IUD), is a reversible method. An IUD is a small device, placed inside the uterus by your doctor to prevent pregnancy. Two types of IUDs are available: a hormone-releasing IUD and a copper-containing IUD.Hormonal methods:
Hormonal methods may prevent pregnancy by delaying or preventing ovulation, creating changes to the cervical mucus and/or creating changes to the uterine lining.Options for hormonal methods:
- A hormone-releasing IUD is implanted into the uterus by your doctor for continuous contraception.
- A long-acting injection containing hormones is given every 3 years.
- A patch is worn on the skin, which releases hormones. It is worn for 3 weeks, removed for 1 week, then a new patch is applied.
- A hormonal vaginal ring is inserted into the vagina. It is worn for 3 weeks, removed for 1 week, then a new ring is inserted.
- Oral pills taken daily can contain a single or a combination of hormones.
Barrier methods:
Common barrier methods include the male condom and the female condom, which prevent sperm from entering the woman’s body. Other available options are a diaphragm or cervical cap, a sponge and spermicides. There is a wide range of options for birth control. A healthcare provider will be able to discuss what works best for you, according to your individual needs.Does Walgreens offer Birth Control?
Walgreens offers a range of birth control options to meet your needs. You can get prescription birth control online through our Virtual Healthcare services, or choose an over-the-counter option like Opill, available without a prescription at Walgreens.com.

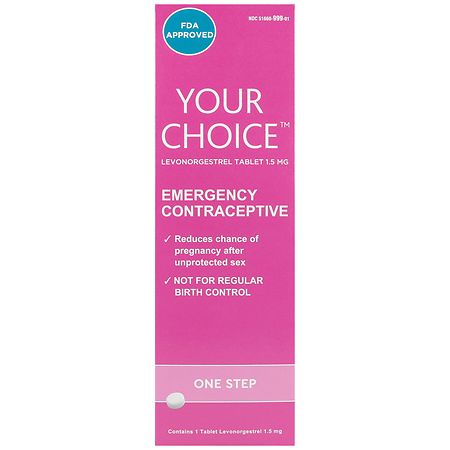
Emergency contraception: what to know
What is emergency contraception?
Emergency contraception (EC) is used as a back-up birth control method to prevent pregnancy in the event of unprotected sex, sexual assault or a contraceptive failure, such as a condom breaking. This includes oral medication options and an intrauterine device.
What are some types of emergency contraception?
Some types of emergency contraception include intrauterine devices (IUDs), over-the-counter oral contraceptive pills and prescription combined estrogen and progestin pills. Examples of the over-the-counter contraceptive pills include levonorgestrel (Plan B One-Step) and ulipristal (ella).
What is the emergency contraceptive pill?
Emergency contraceptive pills are hormone-containing pills that are used to prevent pregnancy after unprotected sex, a missed contraceptive pill or if another contraception method is compromised (e.g., a condom breaks, IUD device falls out). There are two FDA-approved over-the-counter emergency contraceptive pills (ECPs) available: ulipristal acetate (ella) and levonorgestrel (e.g., Plan B One-Step, Take Action).
Emergency contraceptive pills help prevent pregnancy by preventing or delaying ovulation. They do not terminate a pregnancy. They also do not protect against sexually transmitted infections.

A guide to: Emergency contraception
Contraceptives are medicines and devices that reduce the risk of pregnancy. While most contraceptives are used before intercourse occurs, there are medications and devices that can help reduce the risk of pregnancy after sex has occurred. These are known as emergency contraceptives.
Continue reading Opens in a new tab
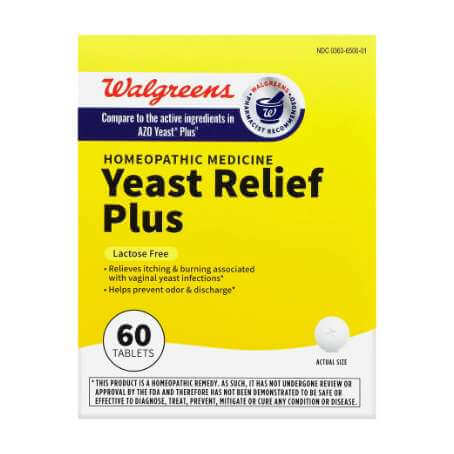
Is it a yeast infection?
What is a vaginal yeast infection?
Vaginal yeast infections, also called vaginal candidiasis, are fungal infections that can cause vaginal irritation and soreness, a thick, white, odorless vaginal discharge with a cottage cheese appearance and an intense itchiness of the vagina and/or vulva. Vaginal yeast infection may also cause pain or discomfort when urinating or during sexual intercourse. Medications can effectively treat vaginal yeast infections. They are extremely common, affecting about 75% of women at some point in their lifetime. They are not sexually transmitted infections.
What are symptoms of a vaginal yeast infection?
Symptoms may include itching and irritation in the vagina or vulva, a burning sensation (especially during intercourse or while urinating), redness and swelling of the vulva, vaginal pain and soreness, vaginal rash, a thick, white, odor-free vaginal discharge with a cottage cheese-like appearance and/or watery vaginal discharge.
What types of medications are available for vaginal yeast infections?
Over-the-counter and prescription strength antifungal medications can effectively treat vaginal yeast infections. These are short courses of vaginal creams, ointments, tablets or suppositories, usually three to seven days of treatment. Some examples of medications used to treat yeast infections include miconazole (Monistat 3), terconazole or fluconazole (Diflucan). For a complete list of medication options and to understand what medication regimen is right for you, speak to a healthcare provider.
Over-the-counter yeast infection solutions
Find relief that’s right for you

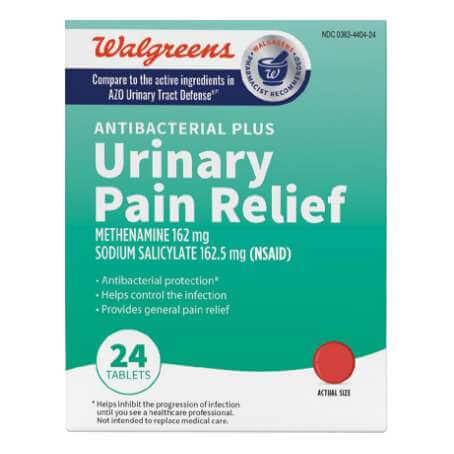
Understanding UTIs
What is a UTI (Urinary Tract Infection)?
A urinary tract infection (UTI) is an infection to any part of the urinary tract, which can include your kidneys, bladder and urethra (the tube that that allows urine to leave your bladder and exit your body). UTIs can occur when bacteria enters the urethra and spreads to the bladder. There are two types of UTIs: the most common type is a bladder infection; the other type is a kidney infection which is less common. UTIs are typically treated with antibiotics. A Walgreens Virtual Healthcare provider can help you decide which treatment is right for you.
How do I know if I have a UTI?
Symptoms of the most common type of UTI, a bladder infection, may include pain or burning while urinating, frequent urination, feeling the need to urinate despite having an empty bladder, bloody urine or pressure or cramping in the groin or lower abdomen. It may also be possible to have a UTI without any symptoms at all. Symptoms such as fever, chills or severe fatigue may be a sign of a more serious infection such as a kidney infection and should be evaluated by a healthcare provider.
What medications are commonly prescribed for UTIs?
UTIs are typically treated with antibiotics. Nitrofurantoin (Macrobid), trimethoprim-sulfamethoxazole (Bactrim) and cephalexin (Keflex) are some medications that may be prescribed for UTIs. To understand what treatment option is best for you, speak to a healthcare provider.
Over-the-counter UTI relief
Feel better with the right relief
Stay on track with Rx alerts & expert care
Frequently Asked Questions
- What is a vaginal yeast infection?
Vaginal yeast infections, also called vaginal candidiasis, are fungal infections that can cause vaginal irritation and soreness, a thick, white, odorless vaginal discharge with a cottage cheese appearance and an intense itchiness of the vagina and/or vulva. Vaginal yeast infection may also cause pain or discomfort when urinating or during sexual intercourse. Medications can effectively treat vaginal yeast infections. They are extremely common, affecting about 75% of women at some point in their lifetime. They are not sexually transmitted infections.
- What causes vaginal yeast infections?
Yeast infections happen when the balance between good bacteria and naturally occurring yeast (candida) in and around the vagina is disrupted, which causes candida to multiply. This can happen for many reasons, including taking antibiotics, changes in hormones, a weak immune system and uncontrolled blood sugar levels.
- What are symptoms of a vaginal yeast infection?
Symptoms may include itching and irritation in the vagina or vulva, a burning sensation (especially during intercourse or while urinating), redness and swelling of the vulva, vaginal pain and soreness, vaginal rash, a thick, white, odor-free vaginal discharge with a cottage cheese-like appearance and/or watery vaginal discharge.
- What types of medications are available for vaginal yeast infections?
Over-the-counter and prescription strength antifungal medications can effectively treat vaginal yeast infections. These are short-courses of vaginal creams, ointments, tablets, or suppositories, usually three to seven days of treatment. Some examples of medications used to treat yeast infections include miconazole (Monistat 3),terconazole, or fluconazole (Diflucan). For a complete list of medication options and to understand what medication regimen is right for you, speak to a healthcare professional.
- Can men get yeast infections?
Although yeast infections are more common in women, men can also get yeast infections, more commonly known as fungal infections. Fungal infections in men lead to jock itch, which can cause itching or a burning feeling in the groin or penile inflammation (balanitis), which involves redness and swelling.
- How can I prevent a yeast infection?
Some basic lifestyle changes may help to prevent yeast infections. These include changing out of wet clothing (like bathing suits or gym clothes) as quickly as possible, as well as wearing cotton underwear and loose-fitting clothes. Avoiding scented feminine products and avoiding hot tubs or very hot baths is also recommended.
Emergency Contraception
- What is emergency contraception?
Emergency contraception (EC) is used as a back-up birth control method to prevent pregnancy in the event of unprotected sex, sexual assault, or a contraceptive failure, such as a condom breaking. This includes oral medication options and an intrauterine device.
- What are some types of emergency contraception?
Some types of emergency contraception include intrauterine devices (IUD), over-the-counter oral contraceptive pills, and prescription combined estrogen and progestin pills. Examples of the over-the-counter contraceptive pills include levonorgestrel (Plan B One-Step) and ulipristal (ella).
- What is the emergency contraceptive pill?
Emergency contraceptive pills are hormone-containing pills that are used to prevent pregnancy after unprotected sex, a missed contraceptive pill, or if another contraception method is compromised (i.e. a condom breaks, IUD device falls out). There are two FDA-approved over-the-counter emergency contraceptive pills (ECPs) available: ulipristal acetate (ella) and levonorgestrel (ex: Plan B One-Step, Take Action).
Emergency contraceptive pills help prevent pregnancy by preventing or delaying ovulation. They do not terminate a pregnancy. They also do not protect against sexually transmitted infections.
- When can emergency contraceptive pills be taken?
Emergency contraception could help to prevent pregnancy if you had unprotected sex, a missed contraceptive pill, or if another barrier method is compromised. It is best to use Emergency Contraceptive Pills as soon as possible. Ella is effective up to 5 days after unprotected sex, whereas levonorgestrel based pills (e.g. Plan B One-Step) is effective for up to 3 days after unprotected sex. The sooner you take it, the more effective these medications will be.
- How effective is the emergency contraceptive pill in preventing pregnancy?
When taken as instructed, emergency contraceptive pills can be effective at preventing pregnancy. For the emergency contraceptive pill, many factors impact the how well they work, including BMI (Body Mass Index) and how soon you take it after unprotected sex.
- Does being overweight or obese change the effectiveness of emergency contraceptive pills?
Yes, being overweight (BMI 25-30) or being a person with obesity (BMI >30) can decrease the effectiveness of emergency contraceptive pills, especially for Plan B One-Step. If you are overweight or obese, it is recommended that you speak to a healthcare professional as they will be best equipped to provide the recommended emergency contraception method based on your individual history.
- Can I use emergency contraception as a regular form of birth control?
No, emergency contraception should not be taken as regular form of birth control.
- Are there side effects to emergency contraceptive pills?
Side effects of emergency contraceptive pills (ECP) can include irregular periods, spotting, fatigue, headaches, dizziness, abdominal pain, nausea and vomiting. If vomiting occurs within 2 hours (for levonorgestrel) or 3 hours (for ulipristal) of taking oral ECP, consider repeating the dose or speaking to a healthcare professional.
Birth Control
- What is birth control?
Birth control, also called contraception, refers to any medicine, method, or device a person uses to prevent pregnancy. Examples include combination oral contraception pills, progestin-only oral contraception pills, transdermal patches, transvaginal rings, diaphragms, and condoms. Not all birth control methods are equally effective, and not all prevent the spread of sexually transmitted infections. A medical professional can help you decide which birth control method is best for you.
- What are the common side effects of birth control pills?
Minor side effects of oral contraceptive pills may include nausea, headaches, spotting or breakthrough bleeding, breast tenderness or enlargement, missed periods, weight gain, mood changes and vaginal discharge.
- How do hormonal contraceptives prevent pregnancy?
Depending on the type of hormone that is used, hormonal contraceptives may prevent pregnancy by stopping or reducing ovulation, thickening the cervical mucus (which helps block sperm from reaching the egg) and thinning the lining of your uterus.
- Can birth control be used for acne treatment?
Some birth control methods are prescribed by doctors to treat hormonal acne. Birth control pills work by controlling the factors that produce excess sebum, which can clog pores and lead to acne.
Some people find their acne improves while on oral contraceptive pills. A healthcare provider can help you decide if this treatment is right for you.
- What does the birth control pill do to your body?
Birth control (BC) pills prevent pregnancy by blocking conception (when sperm fertilizes an egg). BC pills may also prevent pregnancy by preventing or reducing ovulation, cause changes to the uterine lining, and thickening the cervical mucus.
- What are the types of birth control?
There are various types of birth control methods:
Reversible methods:
An intrauterine contraception device (IUD), is a reversible method. An IUD is a small device, placed inside the uterus by your doctor to prevent pregnancy. Two types of IUDs are available: a hormone-releasing IUD and a copper-containing IUD.Hormonal methods:
Hormonal methods may prevent pregnancy by delaying or preventing ovulation, creating changes to the cervical mucus and/or creating changes to the uterine lining.Options for hormonal methods:
- A hormone-releasing IUD is implanted into the uterus by your doctor for continuous contraception.
- A long-acting injection containing hormones is given every 3 years.
- A patch is worn on the skin, which releases hormones. It is worn for 3 weeks, removed for 1 week, then a new patch is applied.
- A hormonal vaginal ring is inserted into the vagina. It is worn for 3 weeks, removed for 1 week, then a new ring is inserted.
- Oral pills taken daily can contain a single or a combination of hormones.
Barrier methods:
Common barrier methods include the male condom and the female condom, which prevent sperm from entering the woman’s body. Other available options are a diaphragm or cervical cap, a sponge and spermicides.There is a wide range of options for birth control. A healthcare provider will be able to discuss what works best for you, according to your individual needs.
UTI Treatment
- What is a UTI (Urinary Tract Infection)?
A urinary tract infection (UTI) is an infection to any part of the urinary tract, which can include your kidneys, bladder, and urethra (the tube that that allows urine to leave your bladder and exit your body). UTIs can occur when bacteria enters the urethra and spreads to the bladder. There are two types of UTIs: the most common type is a bladder infection; the other type is a kidney infection which is less common. UTIs are typically treated with antibiotics. A Walgreens Virtual Healthcare provider can help you decide which treatment is right for you.
- How do I know if I have a UTI?
Symptoms of the most common type of UTI, a bladder infection, may include pain or burning while urinating, frequent urination, feeling the need to urinate despite having an empty bladder, bloody urine, or pressure or cramping in the groin or lower abdomen. It may also be possible to have a UTI without any symptoms at all. Symptoms such as fever, chills, or severe fatigue may be a sign of a more serious infection such as a kidney infection and should be evaluated by a healthcare provider.
- Do I need to visit a physical clinic for a UTI diagnosis?
In-person visits are not always required for the diagnosis of a bladder infection (the most common type of UTI). However, if you are having symptoms that might indicate a more serious infection (e.g. nausea, vomiting, pain below the ribs, fever, chills, or unusual vaginal discharge), or are pregnant or breastfeeding, an in-person appointment with a provider is recommended.
- What medications are commonly prescribed for UTIs?
UTIs are typically treated with antibiotics. Nitrofurantoin (Macrobid), trimethoprim-sulfamethoxazole (Bactrim) and cephalexin (Keflex) are some medications that may be prescribed for UTIs. To understand what treatment option is best for you, speak to a healthcare professional.
- Can I take UTI medications if I'm pregnant or breastfeeding?
If you are pregnant or breastfeeding, we recommend you see a healthcare provider to discuss your individual situation for your care.
- Will a UTI go away without antibiotics?
Most UTIs with symptoms rarely resolve on their own. If you are experiencing UTI symptoms, it is important to seek treatment. Sometimes asymptomatic bacteriuria, which is a UTI without symptoms, can go away on its own but it is always recommended to take next steps under the guidance of a healthcare professional.
Virtual Healthcare Disclaimers
*Currently available in the following states: AL, AZ, CA, CO, CT, FL, GA, IL, IN, KS, KY, LA, MA, MD, MI, MN, MO, NC, NJ, NV, NY, OH, OK, PA, SC, TN, TX, VA, WA, WI. Chat or video visit, varies by state.
Based on national averages. Actual times may vary.
Labcorp and Quest staff are not associates, employees and/or agents of Walgreen Co. or any Walgreens subsidiary or affiliated company. Lab service will be a separate fee, price may vary.
Prescription based on medical evaluation and not guaranteed.
Walgreens-affiliated medical practices are independently owned and operated by licensed physicians who provide services using the Walgreens virtual care program telehealth platform. For more information about the relationship between Walgreens and the medical practices click here.
Walgreens Health Medical Group California P.C. is a California professional medical corporation utilizing the fictitious name “Walgreens Health Medical Group California P.C.” pursuant to Cal. Bus. & Prof. Code § 2415. To view the Fictitious Name Permit click here.